It is an educational platform aim to provide information on i. veins. How to achieve the possible symptomatic, functional and cosmetic outcome by different treatments to the needs of individuals with venous problem. ii. Thyroid diseases, parathyroid, goiter, thyroid cancer, etc... 這是一個教育博客,提供教育關於腿部靜脈曲張及蜘蛛網血管問題,提供各類針對腿部靜脈的治療技術,包括微創靜脈腔內激光及射頻、超聲波導引注射、及外科手術等等。另提供甲狀腺, 甲狀腺亢進, 甲狀腺癌, 甲狀腺腫大, 甲狀腺腫瘤, 甲狀腺素, 甲狀腺 症狀, 甲狀腺素低, 甲狀腺素高, 甲狀腺結節, 甲狀腺醫生, 甲狀腺檢查教育
2020年6月11日 星期四
「有得坐」為何這麼困難?
工作上的長期站立,對員工健康上有壞影響,這個很多人都知。但現實環境中,願意為員工提供適當的設施及安排,去減少工作上不必要站立的商戶,仍屬少數。
筆者早前在快活谷獅子會的支持下,訪問了千多位飲食、零售及服務業的從業員,發現八成以上每天站立時間多於7小時,而有機會坐下的次數少於3次,只有少於兩成的商舖有作出安排去減少站立。大家到百貨公司、酒樓逛逛,相信也能看到這情況的嚴重性。
很多人會覺得,這只是勞資問題,只要老闆明白事理,寬宏大量,批准員工坐坐,問題便能解決。勞工處及職業安全局,在這方面已經印過小冊子,拍過短片,向員工及僱主們宣傳,但情況仍沒甚麼改善。筆者跟僱主們了解過,發現他們也不一定是無良的,很多老闆不是不想員工坐,而是害怕得失客人;顧客走進商舖、食肆,若發覺員工是坐著的,會覺得招呼不周,紀律散漫,對該公司起壞印象,影響其商譽。愈是高級的商舖食肆,這情況愈是嚴重。
因此問題的持份者,是老闆、員工及顧客三方的,而顧客的取態,才是問題的根源。若有一天,顧客走進商店、食肆,看到員工「有得坐」,會認為這是健康商戶、良心老闆的表現,而留下正面的印象;員工亦因為「有得坐」,工作沒有那麼疲累不適,態度更好更投入,招呼客人也更起勁,顧客自然樂於再次幫襯;生意好的話,老闆也樂於繼續讓員工「有得坐」!這是三贏的局面!
因此首先要改變的,是顧客對員工「有得坐」的看法,這是文化的改變,也是最困難的!筆者因工作關係,處理很多長期站立引起的血液循環問題,發覺要治本,就要改變這文化。
作者為外科專科醫生謝卓華
資料來源: AM730
以上所提供的資訊僅作為教育及參考用途,如果你有任何醫療問題,
應向醫生查詢,而不應單倚賴以上提供的資料。
標籤:
外科,
外科專科,
外科專科醫生專科醫生,
謝卓華,
Dr Chad Tse,
Dr Chad Tse Cheuk-wa
位置:
香港
2019年10月10日 星期四
Why DVT can strike anyone, any time and how to avoid a killer blood clot (2)
The first documented case of DVT was reported during the middle ages.
In 1271, a 20-year-old Norman cobbler complained of pain in his lower
leg. A visit to the tomb of canonised King Louis IX was advocated, where
the cobbler massaged dust into his leg.
Subsequent DVTs were diagnosed in pregnant and postnatal women, believed to be the consequence of “evil humours” during pregnancy and post-delivery – meaning a build-up of unconsumed breast milk.
During the first world war, exhausted young soldiers in the trenches suffered from blood clots in their legs, caused by sleeping upright in chairs, their legs beneath them. Today’s taxi and bus drivers are at risk as they sit immobile for long stretches.
Tse says the incidence of DVT among Hongkongers is on the rise. “Overall annual incidences of thromboembolic disease in Hong Kong is 30 per 100,000 of the population; hospital mortality rates associated with DVT are 7.3 per cent.”
The US Centres for Disease Control and Prevention suggests the incidence is higher in America – one to two per 1,000.
One-third of people with DVT or a pulmonary embolism will have a recurrence within 10 years; 10 per cent to 30 per cent of people will die within one month of diagnosis. In the US, one person is diagnosed with DVT every minute, and a sufferer dies as a result of its complication, pulmonary embolism, every six.
Among those with DVT, half will have long-term complications (post-thrombotic syndrome) – as I do: a nagging pain presents in my right calf after prolonged standing or exercise due to enduring damage to valves in the vein.
Flying isn’t the only cause of DVT, and not all people who fly long-haul will develop it. Given the frequency of air travel today, though, it’s a risk we all need to take more seriously. I certainly do: I drink lots of water – “two litres during a seven-hour flight because the atmosphere in the cabin means you dehydrate 20 per cent faster”, my surgeon said.
This means I can’t help but walk up and down the aisle to get my blood circulating, as I get up to use the loo every hour, and instead of skinny jeans I wear toe-to-groin surgical stockings.
Air travel isn’t as sexy as it used to be.
2. Raise and lower your toes while keeping your heels on the floor
3. Tighten and release your leg muscles
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
Subsequent DVTs were diagnosed in pregnant and postnatal women, believed to be the consequence of “evil humours” during pregnancy and post-delivery – meaning a build-up of unconsumed breast milk.
During the first world war, exhausted young soldiers in the trenches suffered from blood clots in their legs, caused by sleeping upright in chairs, their legs beneath them. Today’s taxi and bus drivers are at risk as they sit immobile for long stretches.
Tse says the incidence of DVT among Hongkongers is on the rise. “Overall annual incidences of thromboembolic disease in Hong Kong is 30 per 100,000 of the population; hospital mortality rates associated with DVT are 7.3 per cent.”
The US Centres for Disease Control and Prevention suggests the incidence is higher in America – one to two per 1,000.
One-third of people with DVT or a pulmonary embolism will have a recurrence within 10 years; 10 per cent to 30 per cent of people will die within one month of diagnosis. In the US, one person is diagnosed with DVT every minute, and a sufferer dies as a result of its complication, pulmonary embolism, every six.
Among those with DVT, half will have long-term complications (post-thrombotic syndrome) – as I do: a nagging pain presents in my right calf after prolonged standing or exercise due to enduring damage to valves in the vein.
Flying isn’t the only cause of DVT, and not all people who fly long-haul will develop it. Given the frequency of air travel today, though, it’s a risk we all need to take more seriously. I certainly do: I drink lots of water – “two litres during a seven-hour flight because the atmosphere in the cabin means you dehydrate 20 per cent faster”, my surgeon said.
This means I can’t help but walk up and down the aisle to get my blood circulating, as I get up to use the loo every hour, and instead of skinny jeans I wear toe-to-groin surgical stockings.
Air travel isn’t as sexy as it used to be.
Travel tips to prevent DVT
All air travellers, says Tse, should consider the following:- Stand up and walk around every hour or two;
- Consider wearing knee-high (or higher) compression stockings;
- Apart from the stockings, wear loose-fitting, comfortable clothing;
- Avoid medications such as sedative or sleeping pills, and alcohol, which could impair your ability to get up and move around;
- Flex and extend the ankles and knees periodically, avoid crossing the legs or sitting on your legs, and change positions frequently while seated
The US Centres for Disease Control suggests three simple exercises to help keep the blood flowing:
1. Raise and lower your heels while keeping your toes on the floor2. Raise and lower your toes while keeping your heels on the floor
3. Tighten and release your leg muscles
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
2019年10月9日 星期三
Why DVT can strike anyone, any time and how to avoid a killer blood clot (1)
Who has not heard of DVT – deep vein thrombosis? I thought it
happened only in overweight, unfit people over the age of 50, people who
smoked too much, exercised too little and got their comeuppance as they
ate their way through airline meals on seriously long-haul flights.
So when I – under 50 at the time, fit, non-smoker, lean – awoke after being cat-curled in a seat on a six-hour flight with a pain in my right calf, I naturally assumed it was only a cramp. I stretched my skinny-jean clad legs out, said “ouch”, gave it a rub and disembarked, certain I’d walk the soreness off in no time.
Except that I didn’t. Two days later, the deep ache was waking me at night and I resorted to pain medication. A nagging voice in my head began to question whether this was more than a mere cramp. A cautious friend advised a visit to a doctor’s clinic; the doctor examined my legs: no redness, no heat, no swelling – just pain.
“I’m sure it’s not DVT,” he said, “but we can’t take a chance.”
He sent me off to the accident and emergency department, where I had a blood test for D-dimer – a protein fragment from the breakdown of a blood clot. The test indicated I had DVT, confirmed by an ultrasound.
An injection of blood thinners to further break down the clot was plunged into my abdomen so that a bruise bloomed black and as big as my fist. X-rays of my chest followed, to ensure my lungs were clear and three months of anticoagulants were prescribed.
I was appalled. DVT didn’t happen to people like me: the young (ish), the fit, the lean non-smokers. Oh yes, they do, said the vascular surgeon who examined me.
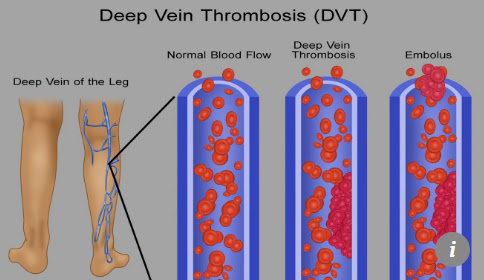
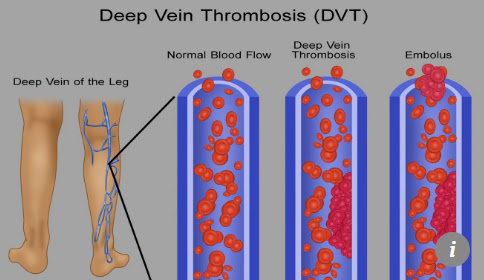
Deep vein thrombosis is the medical term for blood clots in the deep veins of the leg. If a blood clot forms inside a blood vessel, explains Dr Chad Tse Cheuk-wa, a surgeon who specialises in vascular and endovascular surgery at Hong Kong’s Veno Clinic, “it can clog the vessel and keep blood from getting where it needs to go. When that happens, blood can back up and cause swelling and pain.”

DVT is always considered serious, as any clot in a vein “can travel
to other parts of the body and clog blood vessels there”, Tse said.
“Blood clots that form in the legs, for example, can end up blocking
blood vessels in the lungs. This can make it hard to breathe and
sometimes, when they are large, can lead to death.” A blood clot that
travels to the lungs is a pulmonary embolism.
Many things can predispose a person to DVT, including obesity, smoking and age, as well as certain medical conditions, some medications – including birth control pills and hormone replacement therapy (HRT) – and surgery. Dr Tse says prolonged travel – whether by plane, train or automobile – appears to confer a two- to fourfold increase in risk, and taking one long-haul flight a year increases the risk by 12 per cent.
My surgeon said immobility and dehydration are the key reasons flying is a risk – and he warned that “long-haul” can be as short as four hours. Immobility allows the blood in your legs to pool in your calves, and a lack of hydration allows that blood to become “sticky”. The combination of thick, slow-flowing blood is not good.
..........cont'
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
So when I – under 50 at the time, fit, non-smoker, lean – awoke after being cat-curled in a seat on a six-hour flight with a pain in my right calf, I naturally assumed it was only a cramp. I stretched my skinny-jean clad legs out, said “ouch”, gave it a rub and disembarked, certain I’d walk the soreness off in no time.
Except that I didn’t. Two days later, the deep ache was waking me at night and I resorted to pain medication. A nagging voice in my head began to question whether this was more than a mere cramp. A cautious friend advised a visit to a doctor’s clinic; the doctor examined my legs: no redness, no heat, no swelling – just pain.
“I’m sure it’s not DVT,” he said, “but we can’t take a chance.”
He sent me off to the accident and emergency department, where I had a blood test for D-dimer – a protein fragment from the breakdown of a blood clot. The test indicated I had DVT, confirmed by an ultrasound.
An injection of blood thinners to further break down the clot was plunged into my abdomen so that a bruise bloomed black and as big as my fist. X-rays of my chest followed, to ensure my lungs were clear and three months of anticoagulants were prescribed.
I was appalled. DVT didn’t happen to people like me: the young (ish), the fit, the lean non-smokers. Oh yes, they do, said the vascular surgeon who examined me.
Deep vein thrombosis is the medical term for blood clots in the deep veins of the leg. If a blood clot forms inside a blood vessel, explains Dr Chad Tse Cheuk-wa, a surgeon who specialises in vascular and endovascular surgery at Hong Kong’s Veno Clinic, “it can clog the vessel and keep blood from getting where it needs to go. When that happens, blood can back up and cause swelling and pain.”

Many things can predispose a person to DVT, including obesity, smoking and age, as well as certain medical conditions, some medications – including birth control pills and hormone replacement therapy (HRT) – and surgery. Dr Tse says prolonged travel – whether by plane, train or automobile – appears to confer a two- to fourfold increase in risk, and taking one long-haul flight a year increases the risk by 12 per cent.
My surgeon said immobility and dehydration are the key reasons flying is a risk – and he warned that “long-haul” can be as short as four hours. Immobility allows the blood in your legs to pool in your calves, and a lack of hydration allows that blood to become “sticky”. The combination of thick, slow-flowing blood is not good.
..........cont'
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
2018年5月24日 星期四
Why DVT can strike anyone, any time and how to avoid a killer blood clot (2)
The first documented case of DVT was reported during the middle ages.
In 1271, a 20-year-old Norman cobbler complained of pain in his lower
leg. A visit to the tomb of canonised King Louis IX was advocated, where
the cobbler massaged dust into his leg.
Subsequent DVTs were diagnosed in pregnant and postnatal women, believed to be the consequence of “evil humours” during pregnancy and post-delivery – meaning a build-up of unconsumed breast milk.
During the first world war, exhausted young soldiers in the trenches suffered from blood clots in their legs, caused by sleeping upright in chairs, their legs beneath them. Today’s taxi and bus drivers are at risk as they sit immobile for long stretches.
Tse says the incidence of DVT among Hongkongers is on the rise. “Overall annual incidences of thromboembolic disease in Hong Kong is 30 per 100,000 of the population; hospital mortality rates associated with DVT are 7.3 per cent.”
The US Centres for Disease Control and Prevention suggests the incidence is higher in America – one to two per 1,000.
One-third of people with DVT or a pulmonary embolism will have a recurrence within 10 years; 10 per cent to 30 per cent of people will die within one month of diagnosis. In the US, one person is diagnosed with DVT every minute, and a sufferer dies as a result of its complication, pulmonary embolism, every six.
Among those with DVT, half will have long-term complications (post-thrombotic syndrome) – as I do: a nagging pain presents in my right calf after prolonged standing or exercise due to enduring damage to valves in the vein.
Flying isn’t the only cause of DVT, and not all people who fly long-haul will develop it. Given the frequency of air travel today, though, it’s a risk we all need to take more seriously. I certainly do: I drink lots of water – “two litres during a seven-hour flight because the atmosphere in the cabin means you dehydrate 20 per cent faster”, my surgeon said.
This means I can’t help but walk up and down the aisle to get my blood circulating, as I get up to use the loo every hour, and instead of skinny jeans I wear toe-to-groin surgical stockings.
Air travel isn’t as sexy as it used to be.
2. Raise and lower your toes while keeping your heels on the floor
3. Tighten and release your leg muscles
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
Subsequent DVTs were diagnosed in pregnant and postnatal women, believed to be the consequence of “evil humours” during pregnancy and post-delivery – meaning a build-up of unconsumed breast milk.
During the first world war, exhausted young soldiers in the trenches suffered from blood clots in their legs, caused by sleeping upright in chairs, their legs beneath them. Today’s taxi and bus drivers are at risk as they sit immobile for long stretches.
Tse says the incidence of DVT among Hongkongers is on the rise. “Overall annual incidences of thromboembolic disease in Hong Kong is 30 per 100,000 of the population; hospital mortality rates associated with DVT are 7.3 per cent.”
The US Centres for Disease Control and Prevention suggests the incidence is higher in America – one to two per 1,000.
One-third of people with DVT or a pulmonary embolism will have a recurrence within 10 years; 10 per cent to 30 per cent of people will die within one month of diagnosis. In the US, one person is diagnosed with DVT every minute, and a sufferer dies as a result of its complication, pulmonary embolism, every six.
Among those with DVT, half will have long-term complications (post-thrombotic syndrome) – as I do: a nagging pain presents in my right calf after prolonged standing or exercise due to enduring damage to valves in the vein.
Flying isn’t the only cause of DVT, and not all people who fly long-haul will develop it. Given the frequency of air travel today, though, it’s a risk we all need to take more seriously. I certainly do: I drink lots of water – “two litres during a seven-hour flight because the atmosphere in the cabin means you dehydrate 20 per cent faster”, my surgeon said.
This means I can’t help but walk up and down the aisle to get my blood circulating, as I get up to use the loo every hour, and instead of skinny jeans I wear toe-to-groin surgical stockings.
Air travel isn’t as sexy as it used to be.
Travel tips to prevent DVT
All air travellers, says Tse, should consider the following:- Stand up and walk around every hour or two;
- Consider wearing knee-high (or higher) compression stockings;
- Apart from the stockings, wear loose-fitting, comfortable clothing;
- Avoid medications such as sedative or sleeping pills, and alcohol, which could impair your ability to get up and move around;
- Flex and extend the ankles and knees periodically, avoid crossing the legs or sitting on your legs, and change positions frequently while seated
The US Centres for Disease Control suggests three simple exercises to help keep the blood flowing:
1. Raise and lower your heels while keeping your toes on the floor2. Raise and lower your toes while keeping your heels on the floor
3. Tighten and release your leg muscles
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
2018年5月23日 星期三
Why DVT can strike anyone, any time and how to avoid a killer blood clot (1)
Who has not heard of DVT – deep vein thrombosis? I thought it
happened only in overweight, unfit people over the age of 50, people who
smoked too much, exercised too little and got their comeuppance as they
ate their way through airline meals on seriously long-haul flights.
So when I – under 50 at the time, fit, non-smoker, lean – awoke after being cat-curled in a seat on a six-hour flight with a pain in my right calf, I naturally assumed it was only a cramp. I stretched my skinny-jean clad legs out, said “ouch”, gave it a rub and disembarked, certain I’d walk the soreness off in no time.
Except that I didn’t. Two days later, the deep ache was waking me at night and I resorted to pain medication. A nagging voice in my head began to question whether this was more than a mere cramp. A cautious friend advised a visit to a doctor’s clinic; the doctor examined my legs: no redness, no heat, no swelling – just pain.
“I’m sure it’s not DVT,” he said, “but we can’t take a chance.”

He sent me off to the accident and emergency department, where I had a blood test for D-dimer – a protein fragment from the breakdown of a blood clot. The test indicated I had DVT, confirmed by an ultrasound.
An injection of blood thinners to further break down the clot was plunged into my abdomen so that a bruise bloomed black and as big as my fist. X-rays of my chest followed, to ensure my lungs were clear and three months of anticoagulants were prescribed.
I was appalled. DVT didn’t happen to people like me: the young (ish), the fit, the lean non-smokers. Oh yes, they do, said the vascular surgeon who examined me.
Deep vein thrombosis is the medical term for blood clots in the deep veins of the leg. If a blood clot forms inside a blood vessel, explains Dr Chad Tse Cheuk-wa, a surgeon who specialises in vascular and endovascular surgery at Hong Kong’s Veno Clinic, “it can clog the vessel and keep blood from getting where it needs to go. When that happens, blood can back up and cause swelling and pain.”

DVT is always considered serious, as any clot in a vein “can travel
to other parts of the body and clog blood vessels there”, Tse said.
“Blood clots that form in the legs, for example, can end up blocking
blood vessels in the lungs. This can make it hard to breathe and
sometimes, when they are large, can lead to death.” A blood clot that
travels to the lungs is a pulmonary embolism.
Many things can predispose a person to DVT, including obesity, smoking and age, as well as certain medical conditions, some medications – including birth control pills and hormone replacement therapy (HRT) – and surgery. Dr Tse says prolonged travel – whether by plane, train or automobile – appears to confer a two- to fourfold increase in risk, and taking one long-haul flight a year increases the risk by 12 per cent.
My surgeon said immobility and dehydration are the key reasons flying is a risk – and he warned that “long-haul” can be as short as four hours. Immobility allows the blood in your legs to pool in your calves, and a lack of hydration allows that blood to become “sticky”. The combination of thick, slow-flowing blood is not good.
..........cont'
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
So when I – under 50 at the time, fit, non-smoker, lean – awoke after being cat-curled in a seat on a six-hour flight with a pain in my right calf, I naturally assumed it was only a cramp. I stretched my skinny-jean clad legs out, said “ouch”, gave it a rub and disembarked, certain I’d walk the soreness off in no time.
Except that I didn’t. Two days later, the deep ache was waking me at night and I resorted to pain medication. A nagging voice in my head began to question whether this was more than a mere cramp. A cautious friend advised a visit to a doctor’s clinic; the doctor examined my legs: no redness, no heat, no swelling – just pain.
“I’m sure it’s not DVT,” he said, “but we can’t take a chance.”

He sent me off to the accident and emergency department, where I had a blood test for D-dimer – a protein fragment from the breakdown of a blood clot. The test indicated I had DVT, confirmed by an ultrasound.
An injection of blood thinners to further break down the clot was plunged into my abdomen so that a bruise bloomed black and as big as my fist. X-rays of my chest followed, to ensure my lungs were clear and three months of anticoagulants were prescribed.
I was appalled. DVT didn’t happen to people like me: the young (ish), the fit, the lean non-smokers. Oh yes, they do, said the vascular surgeon who examined me.
Deep vein thrombosis is the medical term for blood clots in the deep veins of the leg. If a blood clot forms inside a blood vessel, explains Dr Chad Tse Cheuk-wa, a surgeon who specialises in vascular and endovascular surgery at Hong Kong’s Veno Clinic, “it can clog the vessel and keep blood from getting where it needs to go. When that happens, blood can back up and cause swelling and pain.”

Many things can predispose a person to DVT, including obesity, smoking and age, as well as certain medical conditions, some medications – including birth control pills and hormone replacement therapy (HRT) – and surgery. Dr Tse says prolonged travel – whether by plane, train or automobile – appears to confer a two- to fourfold increase in risk, and taking one long-haul flight a year increases the risk by 12 per cent.
My surgeon said immobility and dehydration are the key reasons flying is a risk – and he warned that “long-haul” can be as short as four hours. Immobility allows the blood in your legs to pool in your calves, and a lack of hydration allows that blood to become “sticky”. The combination of thick, slow-flowing blood is not good.
..........cont'
Reference information: SCMP
It is not intended as medical advice to any specific person. If you have any need for personal advice or have any questions regarding your health, please consult your physicians for diagnosis and treatment.
訂閱:
文章 (Atom)


